
Although it is fairly rare, Krabbe’s disease is a particularly devastating diagnosis. It is a genetic condition that destroys the protective coating (myelin) of nerve cells in the brain and throughout the nervous system, resulting in the loss of voluntary and involuntary function in the body. It is a fatal diagnosis which most commonly occurs in children and has no cure. Most cases are diagnosed in infancy and lead to death by the age of two. But SUNY is hoping to change that.
Nadav Weinstock, a fourth-year M.D./Ph.D. student at the University at Buffalo (UB), is conducting research on Krabbe’s disease.
“The only available treatment for Krabbe’s disease is hematopoietic stem cell transplantation [HSCT], which is effective only if delivered before symptoms manifest,” he said. “Unfortunately this provides a dilemma for clinicians, as there is an inconsistency between early indicators of disease and clinical manifestation of the disease. Secure pre-symptomatic diagnosis is necessary to maximize efficacy of HSCT, but also to avoid the serious complications and mortality that can arise from treating children unnecessarily with HSCT.”
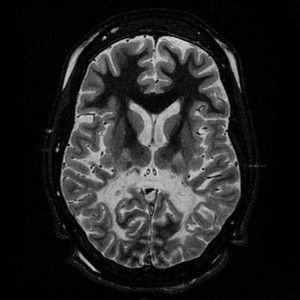 To get around this problem, Weinstock and his colleagues—which include his advisers Laura Feltri, professor of biochemistry at UB and the Hunter James Kelly Research Institute, and Lawrence Wrabetz, professor of neurology and biochemistry and director of the HJKRI—are investigating the concurrent use of positron emission tomography (PET) and magnetic resonance imaging (MRI) to accurately diagnose Krabbe’s disease and other similar diseases before symptoms appear. PET is a test that uses a special type of camera and a radioactive chemical tracer to study organs in the body.
To get around this problem, Weinstock and his colleagues—which include his advisers Laura Feltri, professor of biochemistry at UB and the Hunter James Kelly Research Institute, and Lawrence Wrabetz, professor of neurology and biochemistry and director of the HJKRI—are investigating the concurrent use of positron emission tomography (PET) and magnetic resonance imaging (MRI) to accurately diagnose Krabbe’s disease and other similar diseases before symptoms appear. PET is a test that uses a special type of camera and a radioactive chemical tracer to study organs in the body.
“Combining these two imaging modalities should provide complementary data sets that have the potential to work synergistically in their ability to detect subtle changes in the development of Krabbe’s disease,” said Weinstock, who is using a mouse model to conduct the work. “By studying the biochemical and molecular processes of complex diseases, I hope to find interventions and treatments that can lessen the devastating burden on patient health and well-being.”
Weinstock said that his dissertation project and ultimately his future career as a physician-scientist in the field of pediatric neurology depend on collaboration with researchers in other fields. “By meeting with expert physicists from various institutions as well as clinicians and biomedical researchers, I have begun to grasp the synergy that occurs when experts in different fields come together to work on an important scientific and medical question,” he said.
The project represents a collaboration among Weinstock; Paul Vaska, professor of Biomedical Engineering at Stony Brook University and Brookhaven National Laboratory; Robert Zivadinov, professor of neurology and director of the Buffalo Neuroimaging Analysis Center at UB; and Randy Carter, professor of biostatistics and director of the Population Health Observatory at UB.
Along with the NYS Krabbe Consortium at the HJKRI, these efforts are part of a series of initiatives being developed to maximize the success of the Newborn Screening program for Krabbe Disease and make this deadly diagnosis a thing of the past.



