Various spectrums of light have long been known to kill bacteria. However, it took a recent sit-down between a nurse, an engineer and a microbiologist to apply that particular bit of science to a new device that could save lives and prevent hundreds of thousands of healthcare complications. At Stony Brook University, a multidisciplinary team led by Dr. Annie Rohan is developing a catheter that will use LED lights to reduce the likelihood of catheter-related infection after the device is inserted into a patient’s body.
According to the Centers for Disease Control, patients in U.S. healthcare facilities report over 1.5 million healthcare associated infections annually. Many of these infections are related to the use of indwelling catheters, and can lead to sickness and even death. “It’s a multi-billion dollar-a-year problem,” says Rohan. “Healthcare providers have addressed it with prophylactic antibiotics, hand washing, and other techniques to maintain sterility, but there hasn’t been a product that can successfully reduce infection risk once the device is in the body.”
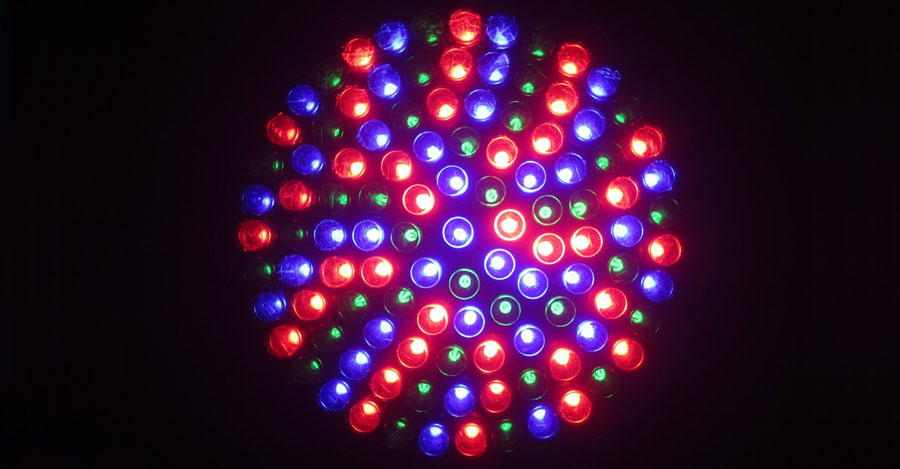
Rohan and her team are investigating spectrums of light which are well established to be bactericidal, but are not expected to damage human tissue. They’ve received an investment from the SUNY Technology Accelerator Fund (TAF) to support proof-of-concept studies that will help them determine the radiance and fluency of light needed to decrease the growth of pathogens.
Because most of these catheters are in very small spaces where they come into direct contact with human tissue, the research team will be testing for cytotoxicity with human cells in the laboratory. Says Rohan, “That’s an extremely important part of these preliminary studies. Before we develop a prototype, we need to be assured that the way we propose to use the light will not damage or change human epithelial cells.”
Developing a clinically acceptable prototype is nowhere near as simple as the science involved, and the genius of this particular project lies in who’s been invited to work on the problem. The study evolved when Dr. Lee Xippolitos, Dean of Stony Brook School of Nursing, introduced Rohan to Charles Davis, a student in the accelerated Registered Nurse Baccalaureate Program who had received a doctorate in materials engineering twenty years earlier.
Like many nurses, he identified a clinical problem and had a great idea to solve it. It was logical that Xippolitos identify Rohan, a dual-certified nurse practitioner with over 25 years of hospital and critical care experience, from among the faculty for the project. Together, Xippolitos, Rohan and Davis were able to take the idea to the next level.
Xippolitos encouraged the pair to seek out collaborators in the university. Using her referral, they connected with Dr. David Thanassi, a Professor in the Department of Molecular Genetics and Microbiology and the Center for Infectious Diseases. Dr. Thanassi’s laboratory works with bacteria that cause urinary tract infections, and these bacteria are particularly problematic for patients with catheters. Under Thanassi’s supervision, laboratory specialists and graduate students supply a continuous stream of data to inform the prototype. Through the Office of Technology, Licensing, and Industry Relations, Rohan and Davis identified a corporate co-sponsor, Michael Bielski, president of DevTech Partners, who was able to identify an expert in catheter product prototyping.
But it is the nursing component that the team believes is both revolutionary and essential to the project’s success. Says Rohan, “The best of technology will go by the wayside if it’s not clinically acceptable. It is imperative that providers – especially nurses – be involved in the development of systems and products that they will need to use. Involving nurses who regularly use these types of devices will go far in assuring that the product is developed with clinical acceptability and usability in mind.”
A microbiologist or engineer, for instance, wouldn’t necessarily know how to address ways to make the catheter both comfortable for patients and easy for providers to use. “Often these devices are designed by people who have a broad – but not specific – understanding of how they will be used in practice,” says Rohan. “Sometimes, it is a very simple design adjustment that makes a world of a difference in terms of clinical acceptability and usability. Bringing nurses into the picture early in the project design phase may be the missing link in how to develop a product that can successfully reduce infection risk.”
Rohan sees these types of multidisciplinary collaborations as a big step forward in solving resistant clinical problems. “Above all,” she adds, “bona fide collaboration is what is important.”



